
Pigmentation & Discolouration
Age Spots Discolouration Hidden Causes of Chronic Melasma Hormonal Pigmentation / Melasma Pigmentation Overview PIH Poikiloderma of Civatte Sun Damaged Skin Why Melasma is Difficult to Treat Why the Sun is Stronger in SASensitive & Reactive Skin
Eczema (Dermatitis) Ingrown Hairs - Razor Bumps Perioral Dermatitis Rosacea / Red Skin Sensitive SkinSkin Concerns in Dark Skin Types
Acne in Dark Skin Dermatosis Papulosa Nigra (DPN) Melasma / Pigmentation In Dark SkinSkin Lesions & Growths
Keloids Onychomycosis (Nail Fungus) Pre-Cancerous Skin Lesions Scars & Scar Removal Sebaceous Hyperplasia Skin Tags Syringoma Warts Wound HealingGeneral Skin Health & Types
7 Sins of Skin Ageing Four Primary Skin Types PCOS and Your Skin Zombie CellsFace, Neck & Chest
Lax / Loose Skin Prejuvenation Sagging Face Skin & Ageing Sunken Cheeks Volume Loss WrinklesLower Face & Mouth
Ageing Lips Double Chin Downturned Mouth Marionette Lines Nasolabial Folds Smoker's LinesUpper Face & Eyes
Bunny Lines Eye Bags Eye Wrinkles / Crow's Feet Sagging Brows Under Eye Dark CirclesAgeing Skin & Conditions
Ageing Décolleté Ageing Hands Ageing Neck Spider Veins Stretch Marks (Striae)Botulinum Toxin Injections
Botox ® & Dysport ® Botulinum Toxin by Decade Brow Lift Palmar Hyperhidrosis Reasons Botulinum Toxin Might Wear Off Too Soon Treatment for Gummy Smile Treatments for Bruxism / TMJ Underarm HyperhidrosisBiostimulators
Biorevitalisation Biostimulation Overview HArmonyCa Profhilo® Revanesse® Pure™ Sculptra Skin BoostersDermal Fillers
Dermal Fillers Juvederm by Allergan Restylane by Galderma Revanesse® by Prollenium® The Science Behind Revanesse®Targeted Filler Treatments
3D Liquid Facelift Hand Rejuvenation Jawline Reshaping Lip Enhancement Magic Needle Mesolift MD Codes™️ Nefertiti Contour Neck LiftInjectable Mesotherapy
Cecarrelli Fat Lipolysis Fat Burning Injections Mesotherapy Mesotherapy for Eye Bags Platelet-Rich Fibrin (PRF) Vampire Facial (PRP)Subcision
Subcision for Acne ScarsCutera
Acutip 500™ CO2 Laser Resurfacing Contact Yag Cutera Lasers Laser Genesis™ Rejuvenation Laser Hair Removal Laser Vein Removal Long Pulsed ND:Yag ND:Yag Skin Tightening Pearl Fractional Pearl Fusion Pearl™ Rejuvenation Titan® Skin TighteningRadiofrequency
Accent ™ Endymed 3Deep RF Tightening Exilis Elite Heat & Sound Technology Lavatron Multipolar vs Monopolar Slimlux Face & Body TitaniaSignature Treatments
Acne & Rosacea Facial Growth Factor–Induced Microneedling Microtox Glow Facial Nasolabial Lift Treatment Star Gaze Eye TreatmentChemical Peels
Chemical Peels Overview Dermaplaning Eye Peel Treatment Intense Peels & Laser Peels MesoBrite™ MicrodermabrasionBody Shaping & Contouring
Body Contouring Carboxytherapy for Body Cellulite Solutions Cryolipo Fat Freezing Endymed ContourWeight Loss Solutions
InBody Analysis Renewal Institute Diet (RID) Shape Up Weight Loss and Chronic Health Why Lifestyle MattersHair & Scalp Solutions
Carboxytherapy for Hair Loss Mesotherapy for Hair Loss Microneedling for Hair Loss
Melasma shows up when several different factors team up to over‑produce pigment in your skin. Even a little sun can "wake up" melanocytes (the cells that make colour), while hormone shifts—like those during pregnancy or from birth control, can push them into overdrive.
Treating melasma is never a one-and-done affair; its stubborn nature stems from multiple layers of complexity that must be addressed simultaneously. In the bullet points below, we'll explore each of these challenges so you can see why a broad, targeted approach is essential for lasting results.
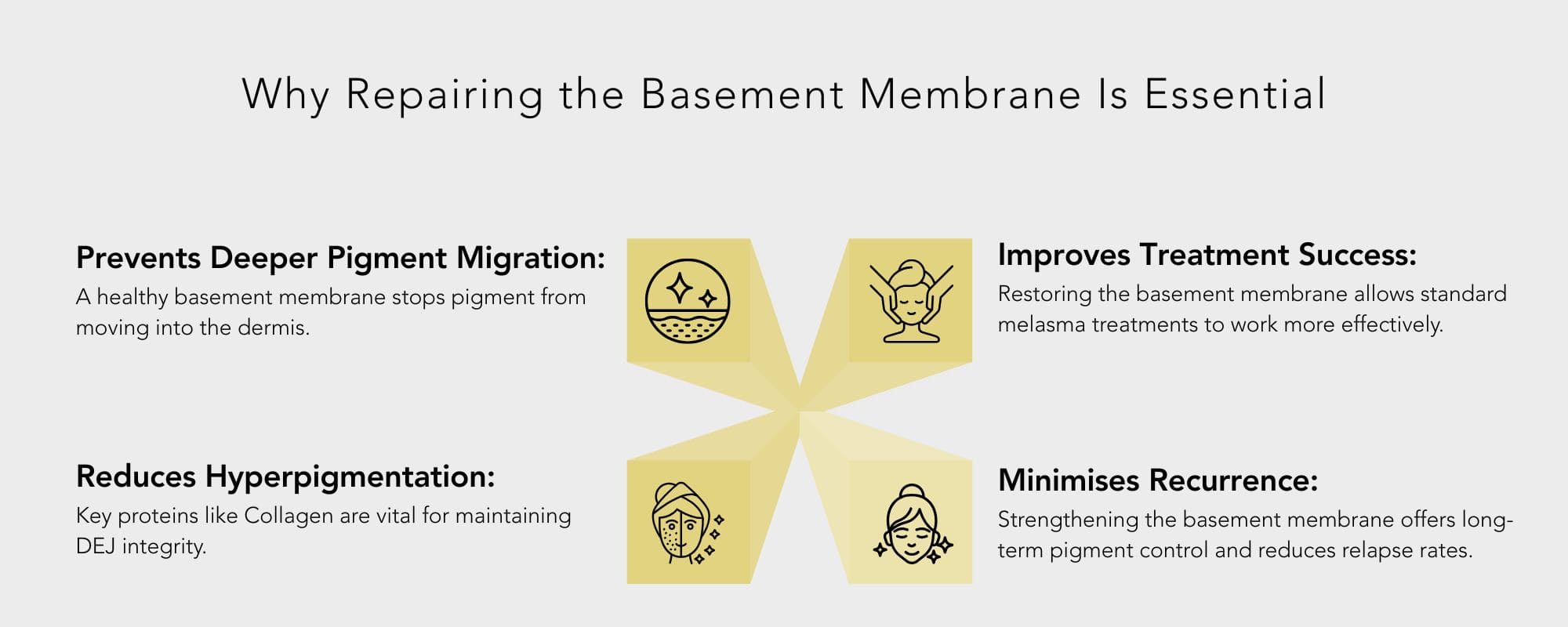
When the basement membrane becomes damaged, melanocytes and pigment particles can penetrate deeper into the dermis, forming pendulous melanocytes. This dermal pigmentation is far more challenging to treat than superficial epidermal pigmentation.
Methylation acts like tiny switches on our DNA, quietly turning genes on or off without changing the genetic code itself. In melasma, these switches become stuck in the "on" position for pigment-making genes, causing melanocytes to produce excess pigment and flood the skin with colour. Sunlight can flip even more of these switches, deepening the tint. Still, treatments such as retinoic acid, niacinamide, and mineral-rich sunscreens work to reset them—soothing oxidative stress and gently coaxing those overactive switches back toward balance.
Slow bowel motility prolongs oestrogen recirculation and raises systemic inflammation—both of which can indirectly fuel hyperpigmentation.
Melasma isn't just about excess pigment — your blood vessels play a significant role, too. Understanding the vascular component helps explain why topical treatments alone may not be enough. Treatments that also target inflammation and blood vessel overgrowth can offer better, longer-lasting results. Here's how increased vascular activity contributes to stubborn pigmentation:
Sun exposure is a primary trigger of melasma and can do more than darken the skin. UV rays can increase blood vessel activity in the skin, potentially worsening pigmentation. This happens in a few ways:
This is why daily sun protection is essential when treating melasma, especially when increased vascularity is a contributing factor.
Hormones play a significant role in the development of melasma, particularly in changes in blood vessels and increased pigmentation.
Emerging research suggests a connection between chronic pigmentation, such as melasma, gut imbalances, including leaky gut syndrome, and inflammation. Poor gut health can lead to increased systemic inflammation, contributing to hormonal imbalances and oxidative stress, thereby exacerbating hyperpigmentation.
Probiotics, prebiotics, anti-inflammatory foods, and eliminating gut disruptors like gluten, dairy, and sugar may help reduce flare-ups and improve skin clarity over time.
Melasma's resilience reflects the many layers of our skin and body, from the skies above to the currents within, and calls for more than a single remedy. At Skin Renewal, we blend science and empathy, guiding you through a personalised plan that unites sun-smart habits, targeted treatments and holistic support. Together, we'll illuminate each challenge, layer by layer, transforming persistent patches into a canvas of confidence and allowing your true radiance to shine through.
Treatments for Melasma are available in Gauteng at the Morningside, Parkhurst, Rosebank, Bedfordview, Fourways, West Rand, Irene, Waterfall, Irene, Lynnwood and Brooklyn clinics, as well as in the Western Cape at Cape Quarter, Claremont, Constantia, Century City, Stellenbosch, Paarl and Willowbridge clinics, and Kwa-Zulu Natal at the Ballito, Durban and Umhlanga clinics.
Melasma typically appears as brown or greyish patches on areas of the face, such as the cheeks, forehead, upper lip, and chin. The pigmentation is usually symmetrical and can vary in size, often triggered by sun exposure or hormonal changes.
To prevent melasma from spreading, it's essential to wear a broad-spectrum sunscreen with SPF 50+ every day, avoid prolonged sun exposure, and use products containing ingredients like Vitamin C and tyrosinase inhibitors. Managing stress and maintaining hormonal balance can also help reduce the spread of melasma.
While there is no direct link between specific foods and melasma, diets high in processed sugars, dairy, and inflammatory foods can contribute to skin inflammation, potentially worsening pigmentation issues. A diet rich in antioxidants, such as fruits, vegetables, and foods high in omega-3, can promote healthy skin.
Melasma can fade over time, especially if triggered by pregnancy or the use of birth control, but it often requires ongoing treatment and maintenance. It can persist or worsen without proper care, especially with continued sun exposure or hormonal imbalances.
Hormones like oestrogen and progesterone are strongly linked to melasma. These hormones increase during pregnancy, when using oral contraceptives, or during hormone replacement therapy (HRT), which can trigger or worsen melasma.
Due to its chronic nature and deep pigmentation, melasma can be challenging to treat. To see noticeable improvements and prevent recurrence, a combination of professional treatments, consistent sunscreen use, and long-term skincare management is required.
Treatments for Melasma are available in Gauteng at the Morningside, Parkhurst, Rosebank, Bedfordview, Fourways, West Rand, Irene, Waterfall, Irene, Lynnwood and Brooklyn clinics, as well as in the Western Cape at Cape Quarter, Claremont, Constantia, Century City, Stellenbosch, Paarl and Willowbridge clinics, and Kwa-Zulu Natal at the Ballito, Durban and Umhlanga clinics.
Melasma typically appears as brown or greyish patches on areas of the face, such as the cheeks, forehead, upper lip, and chin. The pigmentation is usually symmetrical and can vary in size, often triggered by sun exposure or hormonal changes.
To prevent melasma from spreading, it's essential to wear a broad-spectrum sunscreen with SPF 50+ every day, avoid prolonged sun exposure, and use products containing ingredients like Vitamin C and tyrosinase inhibitors. Managing stress and maintaining hormonal balance can also help reduce the spread of melasma.
While there is no direct link between specific foods and melasma, diets high in processed sugars, dairy, and inflammatory foods can contribute to skin inflammation, potentially worsening pigmentation issues. A diet rich in antioxidants, such as fruits, vegetables, and foods high in omega-3, can promote healthy skin.
Melasma can fade over time, especially if triggered by pregnancy or the use of birth control, but it often requires ongoing treatment and maintenance. It can persist or worsen without proper care, especially with continued sun exposure or hormonal imbalances.
Hormones like oestrogen and progesterone are strongly linked to melasma. These hormones increase during pregnancy, when using oral contraceptives, or during hormone replacement therapy (HRT), which can trigger or worsen melasma.
Due to its chronic nature and deep pigmentation, melasma can be challenging to treat. To see noticeable improvements and prevent recurrence, a combination of professional treatments, consistent sunscreen use, and long-term skincare management is required.







